Development Community (Sadc) member states, notably the Democratic Republic of Congo, Zambia, Zimbabwe and South Africa, have registered cases of the viral disease mpox, sending the message that no country, not even Malawi, can count itself out of the woods yet. PATIENCE LUNDA writes on the country’s state of preparedness for the disease.

The Presidential Taskforce on Public Health Emergencies has raised the alert level of mpox, a stance necessitated by the fact that Sadc countries that have never been considered as being at risk of the disease have been registering cases.
Hitherto safe Sadc countries that have been affected include Zambia, Zimbabwe and South Africa.
To date, Malawi has reported 56 suspected mpox cases but, fortunately, they all tested negative.
Zambia recorded its first case of mpox on October 8, with Zimbabwe recording its first two cases on October 13.
All the people that tested positive have a history of travelling to other countries.
Taskforce Chairperson Wilfred Chalamira Nkhoma told Friday Shaker Thursday that while there was no specific treatment for mpox, as it is caused by a virus, the country had put in place requisite measures to manage symptoms in the case of an outbreak.
Nkhoma added that healthcare workers had been trained in how to handle patients that are diagnosed with the disease since it was new to the country.
However, he admitted that the country had not yet fully addressed the animal health aspect of mpox prevention.
The medical expert said taskforce members were engaging officials from national parks.
He added that they were also planning to inspect border points to assess border officials’ readiness for any eventuality.
“We are fine when it comes to diagnosing cases and managing them and we have, this far, had 56 suspects who, when they were tested, were found to be negative. We are ready in case there is a case in the country,” he said.

On his part, Malawi Health Equity Network Executive Director George Jobe emphasised the need for enhanced screening of people at border posts.
He said measures put in place at airports needed to apply to border posts, too.
“We are appealing [to the authorities to ensure] that screening is being done at our border posts because most people travel through our borders because this will be crucial if we are to be spared from mpox cases,” he said.
In mid-August 21 2024, health officials indicated that Malawi had registered two suspected case of mpox virus, barely a week after the World Health Organisation (WHO) declared it a Public Health Emergency of International Concern.
Health Minister Khumbize Kandodo Chiponda said the cases were of people based in Blantyre, one aged 31 years while the other case was of a 17-year-old boy.
Kandodo Chiponda said the man had been isolated at Queen Elizabeth Central Hospital (QECH) while the 17-year-old boy was being managed at home.
Later, she revealed that tests conducted at Malawi Liverpool Wellcome Programme laboratories indicated that the cases were not related to mpox.
At the time, Queen Elizabeth Central Hospital Director Kelvin Mponda indicated that collaboration between stakeholders was proving to be affective.
“We are working hand-in-hand with the Malawi Wellcome Liverpool Programme,” Mponda said.
In a related case, the Ministry of Health recently asked the Department of Animal Health and Production to collaborate with other healthcare officials in protecting people from diseases that are transmitted by animals.
It said this was necessary as there was a growing threat of zoonotic diseases globally.
Deputy head of disease prevention in the ministry, Kondwani Mamba, emphasised the need to enhance proactive measures.
“Many diseases affecting the world originate from animals. We need to work together to find ways to prevent these diseases, ensuring that our country is prepared to respond effectively.” Mamba said.
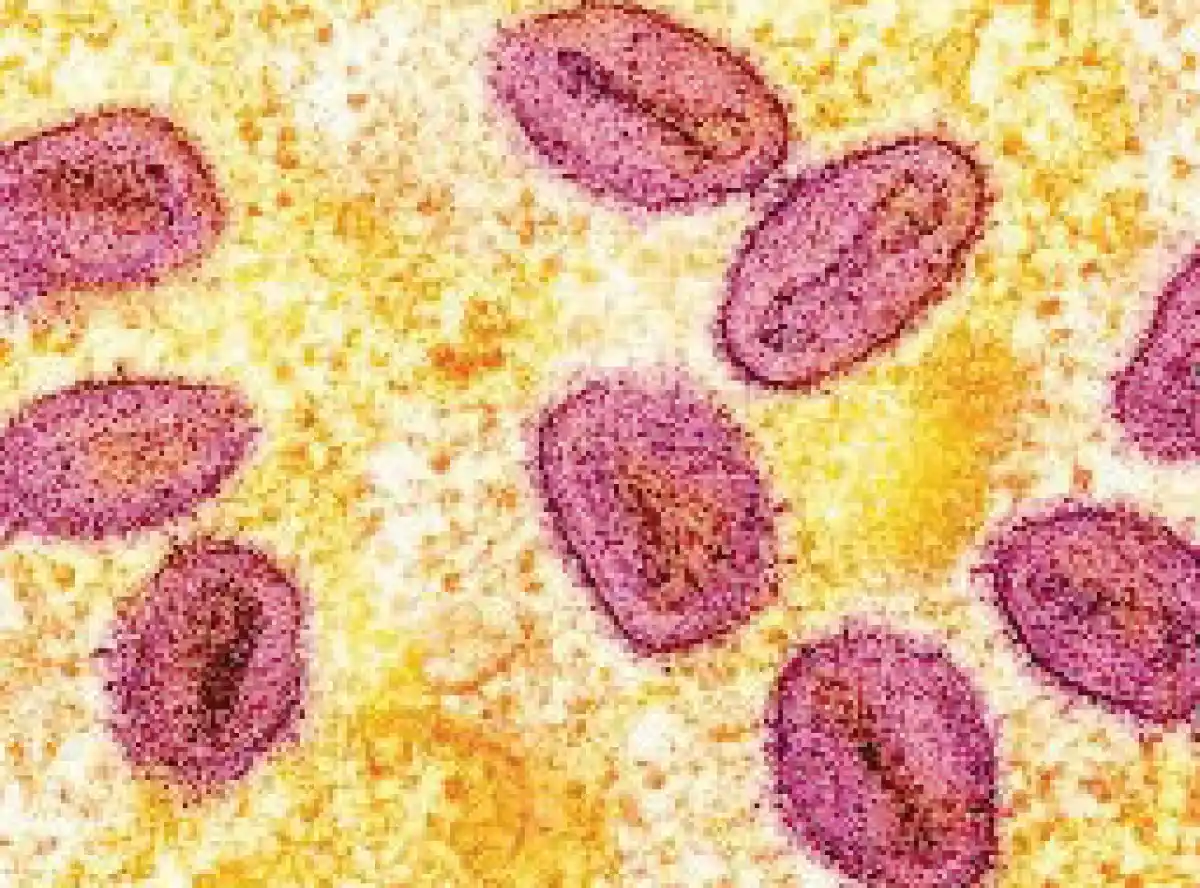
Mpox is an infectious disease caused by the monkeypox virus, commonly abbreviated as MPXV. It can spread from person to person or occasionally from animals to people.
The monkeypox virus was discovered in 1958 in Denmark among monkeys kept for research and the first reported human case of mpox was that of a nine-month-old boy in the Democratic Republic of Congo (DRC) in 1970.
According to WHO, mpox is a viral illness caused by the monkeypox virus, a species of the genus Orthopoxvirus. Two different clades exist: clade I and clade II.
It says common symptoms include a skin rash or mucosal lesions, which can last two to four weeks accompanied by fever, headache, muscle aches, back pain, low energy and swollen lymph nodes.
Furthermore, it says laboratory confirmation of mpox is done by testing skin lesion material by PCR.
“Anyone can get mpox. It spreads from contact with infected: persons, through touch, kissing, or sex; animals, when hunting, skinning or cooking them; materials, such as contaminated sheets, clothes or needles; pregnant persons, who may pass the virus on to their unborn baby,” it says.
In the 2022 outbreak that happened in the United States, more than 32,000 cases were reported, with 58 people dying of the disease.
Since 2023, the DRC has been experiencing an unprecedented outbreak of clade I mpox.








0 Comments